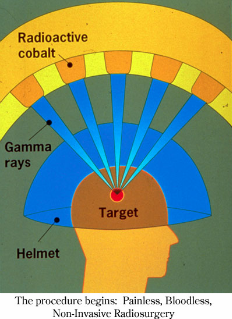
 The Gamma Knife® has set the standard for stereotactic radiosurgery, and has become the primary non-invasive alternative to neurosurgery for various brain tumors and other neurological syndromes. The Gamma Knife® is a dedicated non-invasive stereotactic
radiotherapy machine that replaces the scalpel (or surgery) with a focused array of 201 intersecting beams of high intensity gamma (x-ray) radiation. The gamma radiation is delivered from 201 Cobalt60 sources that provide the ability to precisely
conform the radiation (or x-ray) beams to a tumor's shape, and result in obliteration or destruction of tumors or other brain pathology, replacing the knife of a neurosurgeon. The radiation exposure is brief and only the target tissue being treated
receives a significant radiation dose, while the surrounding normal tissue remains unharmed. Invented in 1968 in Sweden where the first clinical treatment was delivered, the first U.S. unit was installed in 1988 at the University of Pittsburgh. Approved
by the FDA in 1988, it has been used successfully to treat more than 300,000 patients worldwide at state-of-the-art cancer treatment centers (e.g. Mayo Clinic, Johns Hopkins, UCSF.) The majority of treatments are given as an outpatient in a single
session. However, an overnight hospital stay may be occasionally required. The Gamma Knife® offers a non-invasive alternative for many patients for whom traditional brain surgery is not an option and removes the trauma and majority of risks associated
with conventional neurosurgery.
The Gamma Knife® has set the standard for stereotactic radiosurgery, and has become the primary non-invasive alternative to neurosurgery for various brain tumors and other neurological syndromes. The Gamma Knife® is a dedicated non-invasive stereotactic
radiotherapy machine that replaces the scalpel (or surgery) with a focused array of 201 intersecting beams of high intensity gamma (x-ray) radiation. The gamma radiation is delivered from 201 Cobalt60 sources that provide the ability to precisely
conform the radiation (or x-ray) beams to a tumor's shape, and result in obliteration or destruction of tumors or other brain pathology, replacing the knife of a neurosurgeon. The radiation exposure is brief and only the target tissue being treated
receives a significant radiation dose, while the surrounding normal tissue remains unharmed. Invented in 1968 in Sweden where the first clinical treatment was delivered, the first U.S. unit was installed in 1988 at the University of Pittsburgh. Approved
by the FDA in 1988, it has been used successfully to treat more than 300,000 patients worldwide at state-of-the-art cancer treatment centers (e.g. Mayo Clinic, Johns Hopkins, UCSF.) The majority of treatments are given as an outpatient in a single
session. However, an overnight hospital stay may be occasionally required. The Gamma Knife® offers a non-invasive alternative for many patients for whom traditional brain surgery is not an option and removes the trauma and majority of risks associated
with conventional neurosurgery.
A surgical incision and an open skull surgical procedure are not required for Gamma Knife® treatment. Therefore, the attendant risks of open neurosurgical procedures (e.g. hemorrhage, infection, spinal fluid leakage) and general anesthesia are avoided.
In addition, the required inpatient hospitalization and subsequent lengthy rehabilitation period are avoided. The scarring and potential disfigurement that results from open skull surgery is eliminated.
 The Gamma Knife® has been proven safe over the long term and is recognized and covered by insurance plans. There are well over 2,500 peer-reviewed research articles addressing the success of Gamma Knife® treatment, primarily published in neurosurgical
journals. Published reports indicate that the Gamma Knife® may be used as an alternative to standard neurosurgical operations or as an adjuvant (or postoperative) therapy in the treatment of residual or recurrent lesions that remain after conventional
neurosurgical or radiotherapy procedures. Gamma Knife® radiation can be especially useful for those patients who are not suitable for standard surgical techniques due to illness or advanced age. The Gamma Knife is the only feasible treatment in
many neurosurgical cases.
The Gamma Knife® has been proven safe over the long term and is recognized and covered by insurance plans. There are well over 2,500 peer-reviewed research articles addressing the success of Gamma Knife® treatment, primarily published in neurosurgical
journals. Published reports indicate that the Gamma Knife® may be used as an alternative to standard neurosurgical operations or as an adjuvant (or postoperative) therapy in the treatment of residual or recurrent lesions that remain after conventional
neurosurgical or radiotherapy procedures. Gamma Knife® radiation can be especially useful for those patients who are not suitable for standard surgical techniques due to illness or advanced age. The Gamma Knife is the only feasible treatment in
many neurosurgical cases.
The conditions for which Gamma Knife® is considered most effective include brain metastases from a different primary cancer site (e.g. metastatic lung cancer), acoustic neuromas, pituitary adenomas, pineal tumors, craniopharyngiomas, meningiomas,
chordomas, chondrosarcomas, as well as glial tumors including astrocytomas, glioblastoma multiforme, and oligodendrogliomas. In addition, vascular lesions such as arteriovenous malformations (AVMs) are effectively treated by the Gamma Knife®.
Clinical experience also exists in the treatment of functional disorders such as trigeminal neuralgia, intractable pain, Parkinson's disease, essential tremors, and epilepsy. Also, recent favorable results have been seen in the treatment of psychoneural
dysfunctions such as obsessive-compulsive disorder.
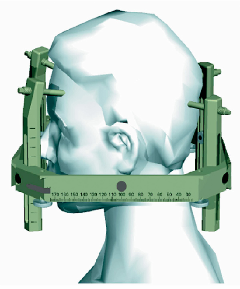
 Initially, a patient who requires Gamma Knife® treatment would undergo a magnetic resonance image (MRI) scan of the brain within one week prior to treatment. On the day of treatment, a neurosurgeon or otolaryngologist performs temporary placement
or fixation of a stereotactic frame to the patient's skull. The head frame is a guiding device, which ensures that the Gamma Knife® beams are focused exactly where the treatment is needed. The frame is made of a lightweight aluminum alloy that
only weighs 3 kilograms, or about 6½ pounds. The frame can be seen on the imaging equipment and provides the physicist with an exact set of coordinates so that the target lesion or tumor is targeted precisely. Before attachment of the frame,
a local anesthetic is given to numb the patient in the locations that the frame will be attached to the skull. This guiding device is left in place until the Gamma Knife® treatment is completed. For brain tumors, a computed tomography (CT) scan
of the brain is then performed with the head frame in place. For treatment of AVMs or other vascular abnormalities, magnetic resonance angiography (MRA) is performed at the same time as the MRI prior to the day of treatment, and an angiogram is performed
in addition to the CT scan after placement of the stereotactic frame on the day of treatment. Depending on the anatomic location of the target lesion or abnormality and its proximity to critical structures, a functional MRI and/or magnetoencephalography
(MEG) study may be performed for functional mapping to assist in delineating important regions of the brain that should be avoided or missed by the x-ray beams.
Initially, a patient who requires Gamma Knife® treatment would undergo a magnetic resonance image (MRI) scan of the brain within one week prior to treatment. On the day of treatment, a neurosurgeon or otolaryngologist performs temporary placement
or fixation of a stereotactic frame to the patient's skull. The head frame is a guiding device, which ensures that the Gamma Knife® beams are focused exactly where the treatment is needed. The frame is made of a lightweight aluminum alloy that
only weighs 3 kilograms, or about 6½ pounds. The frame can be seen on the imaging equipment and provides the physicist with an exact set of coordinates so that the target lesion or tumor is targeted precisely. Before attachment of the frame,
a local anesthetic is given to numb the patient in the locations that the frame will be attached to the skull. This guiding device is left in place until the Gamma Knife® treatment is completed. For brain tumors, a computed tomography (CT) scan
of the brain is then performed with the head frame in place. For treatment of AVMs or other vascular abnormalities, magnetic resonance angiography (MRA) is performed at the same time as the MRI prior to the day of treatment, and an angiogram is performed
in addition to the CT scan after placement of the stereotactic frame on the day of treatment. Depending on the anatomic location of the target lesion or abnormality and its proximity to critical structures, a functional MRI and/or magnetoencephalography
(MEG) study may be performed for functional mapping to assist in delineating important regions of the brain that should be avoided or missed by the x-ray beams.
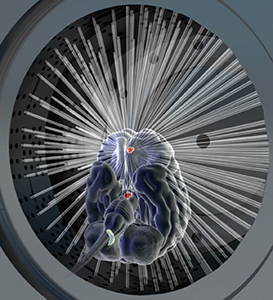
 After all of the appropriate images are imported and registered by a physicist at the treatment planning workstation, the radiation oncologist, neurosurgeon or otolaryngologist, and neuroradiologist define the target area(s) that should receive significant radiation dose as well as the critical structures that should not receive radiation dose. Using sophisticated treatment planning software, the physicist and radiation oncologist then proceed to plan the optimal manner in which to deliver and modify the Gamma Knife® beams such that the target(s) receives the necessary dose and the critical structures are missed. The entire treatment planning process typically takes 1-2 hours. After the treatment planning is completed, the stereotactic frame is then attached to the Gamma Knife® bed to keep the patient's head perfectly still. The treatment is then delivered over approximately 10 to 70 minutes under the direction of the physicist and radiation oncologist. Immediately after treatment delivery is completed, the head frame is removed.
After all of the appropriate images are imported and registered by a physicist at the treatment planning workstation, the radiation oncologist, neurosurgeon or otolaryngologist, and neuroradiologist define the target area(s) that should receive significant radiation dose as well as the critical structures that should not receive radiation dose. Using sophisticated treatment planning software, the physicist and radiation oncologist then proceed to plan the optimal manner in which to deliver and modify the Gamma Knife® beams such that the target(s) receives the necessary dose and the critical structures are missed. The entire treatment planning process typically takes 1-2 hours. After the treatment planning is completed, the stereotactic frame is then attached to the Gamma Knife® bed to keep the patient's head perfectly still. The treatment is then delivered over approximately 10 to 70 minutes under the direction of the physicist and radiation oncologist. Immediately after treatment delivery is completed, the head frame is removed.